Do You Have Any Questions?
Advice after cataract surgery
You are entitled medical leave after your cataract surgery. Usually try to take time off for at least 2 weeks. Depending upon your job, this can be increased as well. The nurse will give you a discharge letter which will also contain information about medications and eye drops.
You may read and watch TV.
Gentle exercises are fine too.
You can go out, but try to avoid crowded and dusty places. Wearing sunglasses when you are outdoors may help to keep your eyes comfortable and less sensitive to light.
You will be given eye drops for about a month to prevent infection and reduce inflammation. Follow your doctor’s instructions carefully. If you need to, ask a family member or friend to help instill the eye drops. If you were to go out, make sure you have access to hand hygiene facilities so that you can clean your hands before you instill your eye drops.
For mild pain, you may take paracetamol. If you have pain that is not relieved by this medicine, call your doctor.
When you sleep, please put on the eye shield given to you for at least 1 week so that you don’t press on the operated eye.
What NOT to do after your cataract surgery
For the first few days, your vision may be blurred, so be careful to avoid falling over or hurting your head or eye.
Do not do gardening for at least 2 weeks.
It is common to experience some eye irritation and discharge after surgery. However, for the first month, refrain from rubbing or touching your eye. Also avoid getting dust or soap water in your eye. Do not swim; do not use a hot tub, visit a sauna or spa. This is because there is a small wound in your eye, and you need to prevent it from getting contaminated.
No matter how small your wound is, try to avoid exerting yourself. Try not to bend over, carry heavy loads or perform strenuous exercises.
Take a break from carrying the grandchildren for 2 to 3 weeks. Let your eye heal.
You may find that your pre-existing spectacles are not right anymore after the cataract operation. This is because the power of your operated eye has changed due to the surgery. Usually the power of the operated eye would stabilize at 1 month after the operation, at which time you can be measured for a new power for your glasses.
Refrain from driving or riding a motorcycle till you are confident that your vision is clear. The law in England states you are not eligible to drive unless you can see a car number plate at 20 meters in good light.
Medications and Diet
For the first few days, please clean the operated eye gently clean your eye with cool boiled water and clean cotton gauze or cotton wool.
Please use the eye drops and medications as the doctor prescribed, even when you feel that your eyes are fine. Do not instill anything else into your eye apart from the prescribed eye drops. Always wash your hands before your instill your eye drops.
Store your eye drops and medications as instructed. Do not keep them for longer than the instructed period as they may become contaminated.
Shake the eye drop bottle before use. Tilt your head back, look up and pull the lower eyelid down. Instill just ONE drop into the eye, avoiding contact with the eye lashes. Wait 5 minutes before instilling a different eye drop.
You can keep to your usual diet. There are no new dietary restrictions following your cataract surgery. Any pre-existing diets should be continued.
When do I see the doctor after surgery?
You will need to return for an eye examination after your surgery. Further appointments are usually after a few weeks to see if the eye is settling well and there is no need for adjustment of eye drops or medication. Keep all your appointments, even if you feel and see well.
When should I call my doctor?
Do not hesitate to contact us should you experience any of the following:
R Redness in the operated eye which worsens over time.
S Sensitivtiy to light increasing
V Visual deterioration progressively
P Pain that is not relieved by medication and eyedrops
- Excessive discharge from the operated eye.
- Sudden onset of flashes or floaters.
Macular diseases
Wet macular degeneration & injection treatment
Wet macular degeneration is a serious condition in which abnormal new blood vessels
grow in between the layers of the retina and choroid (retina is the sensitive film at the back
of the eye). These blood vessels can leak, bleed and cause scarring or water logging
(called odema) in the retina. This leads to loss of vision in the area of the damaged retina.
Unfortunately in most cases, this area, called macula, is responsible for central vision. The
damaged retina caused by these leaky blood vessels ultimately leads to loss of central
vision.
Patients suffering with wet macular degeneration may have central visual loss, blurring of
vision, a grey or black patch in the centre of vision, distortion of straight lines etc. Most
patients will complain of difficulty in reading.
Previous treatments for this eye disease were either not very effective or were very
expensive. Treatments for this kind of eye disease have been developed in the last few
years. One of the most effective and promising treatments is an injection of a anti VEGF
drug into the eye. This may be Eylea (Aflibercept), Lucentis (Ranibizumab) or Avastin
(Bevazicumab). However some patients may benefit from special types of laser treatment
called Argon laser, photodynamic treatment (verteporfin with laser treatment) or even
extensive laser surgery called vitreo retinal surgery.
Intravitreal injections of Eylea (Aflibercept), Lucentis (Ranibizumab) or Avastin
(Bevazicumab) are now routinely given to try and stabilize vision and preserve as much
vision as we can. The goal of treatment is to prevent further loss of vision. Although some
patients will regain vision, the treatment may not restore vision that has already been lost,
and may not ultimately prevent further loss of vision caused by the disease. The damage
in the retina may be reduced by the injections but not totally reversed. Visual loss will be
expected but hopefully not as much if the eye was not treated at all.
The patient usually undergoes tests which include a colour photograph of the retina, a dye
test and a scan of the retina. If there are signs of wet macular degeneration that are
expected to benefit from treatment, then the patient undergoes 3 injections of anti VEGF
treatment (one injection each month for 3 months). The patient then enters an observation
Wet macular degeneration & your treatment options Lucentis, Avastin or Eyelea
Age-related macular degeneration (AMD) is the leading cause of blindness in people over
50 years of age. It is caused by the breakdown of the central portion of the retina (the nerve
layer part of your eye that works like the film in a camera to pick up the picture) called the
macula. The macula is responsible for the fine central vision that’ is needed for driving a
car, reading fine print, recognizing faces, etc.
There are two types of macular degeneration: dry and wet.
In the ‘wet’ form of AMD, abnormal blood vessels grow in the back of the eye.
Sometimes these vessels leak blood or fluid that causes blurred or distorted vision. This
process is also known as choroidal neovascularization (CNV). Without treatment, vision
loss may be quick and severe.
Anti VEGF agents work by blocking vascular endothelial growth factor (VEGF). Blocking or
inhibiting VEGF helps prevent further growth of the abnormal blood vessels that cause
leakage and damage in the eye.
The standard treatment for most forms of wet AMD is intravitreal injections (injections into
the eye). A few forms of wet AMD will require special types of laser as well as intravitreal
injections.
Lucentis and Eyelea treatments are approved by the National Institute of Health & Clinical
Excellence (NICE). As per the NICE guidelines, all patients will not be eligible for treatment
with Lucentis or Eyelea with NHS funding. For patients not meeting the NHS funding
eligibility criteria, patients are often offered treatment with intravitreal Bevacizumab
(Avastin).
Your choices are:
Avastin (Bevazicumab)
Lucentis (Ranibizumab)
Eyelea (Aflibercept)
Risk when anti VEGF agents are given to treat patients with eye conditions:
Most ophthalmologists believe that the risk of these complications for patients with eye
conditions is low.
All 3 medicines are anti VEGF
agents, which are delivered by an
injection into the jelly of the eye.
Known risks are stroke, heart problems and high blood pressure amongst others.
Known risks of intravitreal eye injections:
Infection inside the eye called endophthalmitis.
Inflammation of the eye
Retinal detachment
Cataract formation (clouding of the lens of the eye)
RPE rip ( inward curling of a layer of the retina)
Glaucoma (increased pressure in the eye)
Bleeding
Additional procedures may be needed to treat these complications.
Any of these rare complications may lead to severe, permanent loss of vision.
Patients receiving an injection may experience less severe side effects related to the
procedure. These usually settle down in a day or two with the ointment or drops.
These side effects may include
eye pain caused by scratched cornea ( corneal abrasion)
subconjunctival haemorrhage (bloodshot eye)
vitreous floaters or grey bubbles ( intravitreal air)
irregularity / dryness the cornea (dry eye)
Lucentis treatment
Lucentis is licensed for the treatment of wet macular degeneration and is recommended by
NICE. Currently it is the most commonly used drug for the treatment of wet macular
degeneration.
Eyelea treatment
Eyelea is also licensed for the treatment of wet macular degeneration and is recommended
by NICE. Eyelea is the latest drug to be approved for the treatment of wet macular
degeneration. Studies suggest that less injections of Eyelea may be required for visual
stabilisation compared to Lucentis over a year.
Avastin treatment and “Off Label” Status
Avastin was not initially developed to treat your eye condition. Avastin is approved for the
treatment of metastatic colorectal cancer. It does not have a licence for eye use.
Once a device or medication is approved by the regulatory authorities, physicians may use
it ‘off-label’ for other purposes if they are well informed about the product, base its use on
firm Scientific method and sound medical evidence, and maintain records of its use and
effects. Ophthalmologists all over the world are also using Avastin ‘off-label’ to treat AMD
and similar conditions.
Two large trials (CATT trial in the USA and IVAN trial in the UK) comparing Lucentis and
Avastin shows fairly similar results in treatment of wet AMD.
Avastin is a significantly cheaper drug than Lucentis. There appears to be a slightly higher
risk of infection, stroke or heart trouble with Avastin when compared with Lucentis. The risk
appears to be low when both drugs are compared. However any number of coincidental
life-threatening problems may occur that have no relationship to treatment drugs.
Prospects with Anti VEGF treatment
Approximately 80% of patients are likely to respond to Anti VEGF treatment and their vision
may stabilize. Of these approximately 20% patients may find an improvement in their sight.
Around 20% of patients will not respond and their vision will deteriorate.
Some patients may just need 3 injections while others may need significantly more before
the vision stabilises.
Patient Responsibilities
You should contact your Ophthalmologist if any of the following signs of infection or other
complications develop such as pain, blurry or decreased vision, sensitivity to light, redness
of the eye (compared to immediately after the injection), or discharge from the eye.
You are instructed not to
rub your eyes
swim
use makeup around the eye
gardening for five days after each injection
You should attend-all your post-injection appointment schedules.
Although the likelihood of serious complications affecting other organs of your body is low,
you should immediately contact your GP or visit A&E if you experience abdominal pain,
chest pain, severe headache, slurred speech or weakness on one side of the body and you
should notify these problems to your ophthalmologist.
If you have had an injection and are concerned about a serious complication with redness,
eye pain and decreased vision, please visit your closest eye casualty department. If you are
in central London, please visit Moorfields eye hospital eye casualty.
Wet macular degeneration & injection treatment
Wet macular degeneration is a serious condition in which abnormal
new blood vessels grow in between the layers of the retina and
choroid (retina is the sensitive film at the back of the eye). These
blood vessels can leak, bleed and cause scarring or water logging
(called odema) in the retina. This leads to loss of vision in the area
of the damaged retina. Unfortunately in most cases, this area,
called macula, is responsible for central of vision. The damaged
retina caused by these leaky blood vessels ultimately leads to loss
of central vision.
Patients suffering with wet macular degeneration may have central
visual loss, blurring of vision, a grey or black patch in the centre of
vision, distortion of straight lines etc. Most patients will complain of
difficulty in reading.
Treatments for this kind of eye disease have been developed in the
last few years. One of the most effective and promising treatments
is an injection of a drug into the eye. This may be Lucentis
(Ranibizumab), Avastin (Bevazicumab) or Eylea (Aflibercept).
Previous treatments for this eye disease were either not very
effective or were very expensive. However some patients may benefit from special types of laser treatment called Argon laser,
photodynamic treatment (verteporfin with laser treatment) or even
extensive laser surgery called vitreo retinal surgery.
Intravitreal injections (Lucentis, Avastin or Eylea) are now routinely
used to try and stabilize vision and preserve as much vision as we
can. The goal of treatment is to prevent further loss of
vision. Although some patients may regain some lost vision, the
treatment may not restore vision that has already been lost, and
may not ultimately prevent further loss of vision caused by the
disease. The damage in the retina may be reduced by the injections
but not totally reversed. Visual loss will be expected but hopefully
not as much if the eye was not treated at all.
The patient usually undergoes tests which include a colour
photograph of the retina, a dye test and a scan of the retina. If there
are signs of wet macular degeneration that are expected to benefit
from treatment, then the patient undergoes 3 injections of antiVEGF
treatment (one injection each month for 3 months). The patient
then enters an observation period and will then be offered treatment
only if it is required. This injection is given directly into the eye (in the jelly of the eye), by
an eye surgeon.
The eye will be sore for a while and the vision will be blurred for a
period of time after which it will clear to previous levels.
The chances of stabilization of the vision are upto 80% in patients
with certain types of wet macular degeneration. In approximately
20% the treatment will not work and the vision will drop. The
damage caused by leakage and fluid may be minimised but the
ageing changes cannot be stopped.
In most cases, patients do not have any problems after the
injection. Sometimes the front surface of the eye can get scratched
(corneal abrasion), which can cause eye pain/soreness but settles
down in a day. Rarely, patients can get an infection in the eye,
called endophthalmitis (1% chance), which can cause permanent &
total loss of vision.
Possible complications and side effects of the procedure and
administration of injection treatments include retinal detachment,
cataract formation (clouding of the lens of the eye), glaucoma
(increased pressure in the eye), inflammation (soreness), hypotony
(reduced pressure in the eye), damage to the retina, cornea or lens
(structures of the eye), and bleeding. Another complication called
retinal pigment epithelial rip (inward curling of lining of the retina)
can cause decreased vision in patients with certain types of wet
macular degeneration. Any of these rare complications may lead
to severe, permanent loss of vision.
There is also some evidence emerging suggesting slightly higher
chance of strokes (2%) in patients receiving Lucentis or Avastin.
Summary
Benefits: Possible stabilization of vision
Risks: Frequent injections into the eye which may be painful.
Complications may cause permanent loss of sight. Failure of
treatment may lead to loss of sight
What to expect after your intravitreal injection
You may have received an intravitreal injection of Lucentis / Eylea/ Avastin today. For
some patients an injection can be painful, in some instances it will be felt as a prick.
In almost all instances, after the injection, you will be asked to count fingers. If after the
injection , you feel you cannot see anything please inform the doctor, who may need to
do more tests or perform an additional procedure related to the injection, before he or
she decides you are ok to leave.
Almost all patients will be given an antibiotic drop bottle or antibiotic ointment. This is to
try and reduce the chances of an infection. Please put in the drops 3 to 4 times a day on
the day of injection and then 4 times a day for 3 days after the injection. Some patients
may also be given an eye gel called Viscotears. This is to try and improve the corneal
healing after small scratches or corneal dryness.
You may expect the vision to be blurry for a while after the intravitreal injection. This is in
part due to the injection and also due to the dilation of the pupil. This is expected to get
better in 3 to 4 hours as the drops wear off.
Sometimes a small bubble of air can get into the eye with the injection. It can look like a
small round grey blob in the bottom part of your vision. This is usually harmless and
goes away in 24 to 48 hours.
Sometimes the cornea can get small scratches due to the speculum (the clip that keeps
the eye open during the injection). In such instances, the eye may feel gritty and sore.
You may feel this as soon as the anaesthetic wears off in 20-30 minutes. You may need
to use lubricant gels like Viscotears or Lacrilube to keep the eye comfortable. These are
available in a pharmacy, “over the counter”, without a prescription.
If your eye gets red and painful with decreased vision, this may be a sign of infection. If
you have these symptoms, please attend the eye casualty as soon as possible. Do not
delay to come to any eye casualty, if you suspect an infection.
In the first instance, try to contact Mr Sheikh’s secretary 01737 919000
Local Eye casualty departments are as follows
Moorfields eye hospital, City road, London has a 24 hours casualty
Outside these hours and on Saturday and Sunday, please attend the Eye department at
East Surrey hospital, Redhill.
Diabetic Eye Conditions
Diabetic maculopathy
Diabetes is a condition that can damage many parts of the body including the eyes.
The nerves, blood vessels, kidneys and other organs of the body can get damaged due to
complications of diabetes.
Over time, damage can develop in the blood vessels that supply the central retina (at the back of
the eye). This can lead to vision loss, which can affect distance vision and near vision or fine detail,
such as the small print in a document.
As diabetic retinopathy reaches advanced stages, some of the blood vessels that supply the retina
will become blocked. To compensate for this, the body will start to produce new blood vessels to
restore the supply of blood. These blood vessels may bleed or leak.
As the new blood vessels are unstable and prone to bleeding, they can cause blurred and patchy
vision as the blood obscures your sight. Over time, the bleeding can lead to the formation of scar
tissue. There is a risk that this will pull your retina out of position. This is known as retinal
detachment. Retinal detachment can lead to a darkening of vision, floaters and, if left untreated, a
total loss of vision.
The central part of the retina called macula can also become affected by water-logging and leakage
due to diabetes. This is called diabetic maculopathy and can lead to central visual loss, patchy
vision and inability to see small print etc.
Risk factors
There are a number of risk factors that increase your chances of developing diabetic retinopathy.
Duration of diabetes; the biggest risk factor for diabetic retinopathy is the length of time that you
have lived with diabetes.
Blood glucose level; People with high blood glucose levels are more likely to progress to advanced
diabetic retinopathy.
High blood pressure; People with high blood pressure (hypertension) are likely to progress to
advanced diabetic retinopathy.
- Other risk factors are:
age
family history
African-Caribbean or south Asian origin
obesity
stress
lack of exercise
smoking
excessive alcohol consumption
a high amount of salt in your diet
a high-fat diet
Treatment
For early or moderate diabetic retinopathy the best treatment is good control of diabetes and
control of risk factors including keeping your blood pressure at optimum levels ( around 120/80
mmHg)
Advanced diabetic retinopathy like diabetic maculopathy (with sight threatening features) and
proliferative retinopathy usually require laser treatment.
In advanced proliferative retinopathy, laser treatment may not be possible and a type of eye
surgery called vitreous surgery may be required.
Aim of treatment
Aim of the laser treatment is to keep your vision stable. It is unlikely to improve your vision.
Statistics show 70% stabilization of vision, 15% improved vision and 15% worse vision after focal
laser for diabetic maculopathy.
Laser or injection treatment cannot replace good diabetic control. If your diabetes, blood
pressure and cholesterol remain out of control, laser or injection treatments will fail and you
may lose vision.
Laser treatment
The type of laser treatment used to treat diabetic retinopathy is known as photocoagulation.
Photocoagulation involves using a laser to burn away any abnormal blood vessels or abnormal
retina which may affect the normal retina.
Laser for diabetic maculopathy stabilizes or improves vision in 85% of patients. Approximately 15%
of patients will experience visual loss even after laser treatment for diabetic maculopathy. This is
usually because of progressive damage by diabetes affecting the blood vessels of the retina.
Photocoagulation reduces the risk of severe visual loss over 5 years by 50% in patients with
proliferative diabetic retinopathy.
More than 50% of people who have laser treatment for diabetic retinopathy notice some difficulty
with their night vision, and 3% notice some loss of peripheral vision.
Injection treatment:
Injections can help in certain types of diabetic retinopathy by reducing leakage in the retina.This
type of retinopathy is called diabetic maculopathy. Initial stages of diabetic maculopathy may be
treated with laser. However in some instances or later stages, injections may be more helpful. The
injections of drugs called Ranibizumab (Lucentis®), Bevazicumab (Avastin®), Afiblicept (Eyelea®),
Triamcinolone or Flucinolone acetate (Illuvien®) are usually used depending on circumstances. You
should talk to your doctor about these as each of these will have risks and benefits, which will
need to be considered on a case to case basis.
Seek medical advice if you experience any new eye problems following treatment.
Disclaimer: This information leaflet is produced to help increase awareness regarding diabetic retinopathy. It is not
intended to replace professional medical advice or to provide advice in any special individual circumstance. Please
seek expert medical advice regarding your specific medical condition.
Sources: http://www.cks.nhs.uk/patient_information_leaflet/diabetic_retinopathy
Diabetic retinopathy
Patient information Diabetic Retinopathy
Diabetes mellitus is a condition which affects the regulation of blood glucose in your body.
Diabetes can damage many organs in the body including skin, nerves, kidneys, blood vessels, heart
and eyes.
Sustained and uncontrolled blood glucose levels eventually cause damage to the structures of the
eye called diabetic retinopathy or diabetic maculopathy. These changes can be by an eye doctor
either by special scans and photographs or by examining the eye with special pieces of equipment.
Over time, damage can develop in the blood vessels that supply the retina . This can lead to some
vision loss, which can affect both seeing things clearly at a distance and seeing things in fine detail,
such as the small print in a document.
As diabetic retinopathy reaches its most advanced stage, some of the blood vessels that supply
your retina will become blocked. To compensate for this, your body will start to produce new blood
vessels to restore the supply of blood. These blood vessels may bleed or leak.
As the new blood vessels are unstable and prone to bleeding, they can cause blurred and patchy
vision as the blood obscures your sight. Over time, the bleeding can lead to the formation of scar
tissue. There is a risk that this will pull your retina out of position. This is known as retinal
detachment.
Retinal detachment can lead to a darkening of vision, floaters and, if left untreated, a total loss of
vision.
Risk factors
There are a number of risk factors that increase your chances of developing diabetic retinopathy.
Duration of diabetes; The biggest risk factor for diabetic retinopathy is the length of time that you
have lived with diabetes.
Blood glucose level; The higher the levels of glucose in your blood, the greater your risk of
developing diabetic retinopathy. People with high blood glucose levels are more likely to progress
to advanced diabetic retinopathy.
High blood pressure; People with high blood pressure (hypertension) are likely to progress to
advanced diabetic retinopathy.
Other risk factors are:
age
family history
African-Caribbean or south Asian origin
obesity
stress
lack of exercise
smoking
excessive alcohol consumption
a high amount of salt in your diet
a high-fat diet
Treatment
For early or moderate diabetic retinopathy the best treatment is good control of diabetes and
control of risk factors.
Advanced diabetic retinopathy like diabetic maculopathy (with sight threatening features) and
proliferative retinopathy usually require laser treatment.
In advanced proliferative retinopathy, laser treatment may not be possible and a type of eye
surgery called vitreous surgery may be required.
Laser or injection treatment cannot replace good diabetic control. If your diabetes, blood
pressure and cholesterol remain out of control, laser or injection treatments will fail and you
may lose vision.
Laser treatment
The type of laser treatment used to treat diabetic retinopathy is known as photocoagulation.
Photocoagulation involves using a laser to burn away any abnormal blood vessels or abnormal
retina which may affect the normal retina.
Photocoagulation reduces the risk of severe visual loss over 5 years by 50%.
More than 50% of people who have laser treatment for diabetic retinopathy notice some difficulty
with their night vision, and 3% notice some loss of peripheral vision.
Injection treatment:
Injections can help in certain types of diabetic retinopathy by reducing leakage in the retina.This
type of retinopathy is called diabetic maculopathy. Initial stages of diabetic maculopathy may be
treated with laser. However in some instances or later stages, injections may be more helpful. The
injections of drugs called Ranibizumab (Lucentis®), Bevazicumab (Avastin®), Afiblicept (Eyelea®),
Triamcinolone or Flucinolone acetate (Illuvien®) are usually used depending on circumstances. You
should talk to your doctor about these as each of these will have risks and benefits, which will
need to be considered on a case to case basis.
Seek medical advice if you experience any new eye problems following treatment.
Disclaimer: This information leaflet is produced to help increase awareness regarding diabetic retinopathy. It is not
intended to replace professional medical advice or to provide advice in any special individual circumstance. Please seek
expert medical advice regarding your specific medical condition.
Draft version 1.2 /MUS
Sources: http://www.cks.nhs.uk/patient_information_leaflet/diabetic_retinopathy
Laser treatments and what to expect
YAG capsulotomy advice
YAG laser may be used to create a small opening in a thickened capsule
(membrane), just behind the artificial lens of the eye (after cataract surgery).
There are no special preparations before eye laser treatment. You should eat
normally and take your regularly prescribed medications before surgery.
Nd-YAG laser capsulotomy (laser surgery) is performed in the consulting room or a
special laser room.
Eye drops will be given to dilate the pupil and numb the eye. The treatment is
performed while you are seated in a chair, similar to the one used for regular eye
examinations. You will remain awake and comfortable.
Treatment is usually painless.
The treatment generally takes 5 to 10 minutes after starting the procedure.
Most people will notice improved vision approximately 3-4 hours after the procedure
( if there is no other eye condition affecting the eye or vision)
Almost all patients can expect floaters. These floaters usually settle down after a few
weeks and become less troublesome. Some floaters may take a few months and in
very rare patients remain permanent.
You may expect improvement in vision. In particular the brightness, colour and
contrast should improve.
Post operative medications are usually not required in a significant proportion of
patients. In some patients drops and tablets may be required for a few days after the
laser treatment. This may depend on your individual circumstances and the doctor’s
preference. The surgeon will write you a prescription only if it is required.
There are virtually no restrictions following retinal laser surgery, and you should be
able to resume your normal activities and work schedule the following day.
Disclaimer: This information leaflet is produced to help increase awareness in patient s undergoing laser
treatments. It is not intended to replace professional medical advice or to provide advice in any special
individual circumstance. Please seek expert medical advice regarding your specific medical condition.
YAG iridotomy advice
YAG laser may be used to create a small opening in a the iris (which is the coloured
part of the eye). In simple terms, this creates improved flow of fluids inside the eye
and reduces chances of sudden rise in eye pressure called acute glaucoma. Acute
glaucoma is a serious condition which can cause permanent loss of sight within 48
hours if left untreated.
There are no special preparations before eye laser treatment. You should eat
normally and take your regularly prescribed medications before surgery.
Nd-YAG laser iridotomy (laser surgery to make a hole in the iris) is performed in the
consulting room or a special laser room.
Eye drops will be given to dilate the pupil and numb the eye. The treatment is
performed while you are seated in a chair, similar to the one used for regular eye
examinations. You will remain awake and comfortable.
Treatment is usually painless but some patients can have mild discomfort.
The treatment generally takes 5 to 10 minutes after starting the procedure.
Most patients notice no vision changes following their laser surgery, although there
may be some temporary blurring for a few days or weeks. Some patients may have a
gritty sensation in the eyes for a few days which usually settles down with drops.
It will take several weeks to months before we can tell whether the laser surgery has
been successful.
Post operative medications are usually required. These include drops and
occasionally tablets for a few days after the laser treatment.
There are virtually no restrictions following laser surgery, and you should be able to
resume your normal activities and work schedule the following day.
If the pressure becomes high you may experience, eye pain and redness with
decreased vision. The YAG iridotomy is to try and reduce the chances of such a
pressure rise. If the treatment is successful the chances of a pressure rise are
reduced but not to zero. You can still have an episode of raised pressure in the eye
called acute glaucoma. If this happens please contact the closest ophthalmic eye
casualty to start immediate treatment.
Disclaimer: This information leaflet is produced to help increase awareness in patient s undergoing laser
treatments. It is not intended to replace professional medical advice or to provide advice in any special
individual circumstance. Please seek expert medical advice regarding your specific medical condition.
Retinal laser advice
There are no special preparations before eye laser treatment. You should eat
normally and take your regularly prescribed medications before surgery.
Retinal laser surgery is performed in the consulting room or a special laser room.
Eye drops will be given to dilate the pupil and numb the eye. The treatment is
performed while you are seated in a chair, similar to the one used for regular eye
examinations. You will remain awake and comfortable.
Treatment is usually painless, although some patients may require a numbing
injection for discomfort or sensitivity to the laser light. Patients who have laser
treatment for diabetic retinopathy may experience more discomfort towards the end
of a laser treatment session.
The laser treatment usually takes less than 30 minutes to complete, and you can go
home immediately following surgery.
Arrangements for transportation should be made in advance since you may not be
able to drive right away.
You may expect blurred vision for the rest of the day after laser treatment.
There are virtually no restrictions following retinal laser surgery, and you should be
able to resume your normal activities and work schedule the following day.
Most patients notice no vision changes following their laser surgery, although there
may be some temporary blurring for several weeks to months. In addition, depending
on the condition being treated, some may notice a permanent blind spot or decrease
in peripheral and night vision.
It will take several weeks to months before we can tell whether the laser surgery has
been successful.
Many patients, however, will need more than one treatment to control their eye
problem and prevent further loss of vision.
Disclaimer: This information leaflet is produced to help increase awareness in patient s undergoing retinal
laser. It is not intended to replace professional medical advice or to provide advice in any special individual
circumstance. Please seek expert medical advice regarding your specific medical condition.
Miscellaneous
Questions About
Miscellaneous
Questions About
Floaters
- Floaters are extremely common over the age of the age of 65, with 50% of over 65 experiencing
floaters.
Early stage of floaters can be extremely worrying.
Symptoms
In some cases, the only noticeable symptom is a sudden appearance of a floater.
In most cases, the floater can be preceded by or accompanied by flashing lights.
Symptoms of may include:
discoloured spots (known as floaters that ‘float’ in your field of vision)
Floaters which moves around in your field of vision and may be like a cobweb, a fly, a
tadpole or any other random shape
Flashing lights
Why do floaters form?
Over time, the jelly of the eye undergoes changes. Some parts of the jelly of the eye become
thinner and some other parts become thicker. The jelly which previously was well formed breaks
up and separates from the retina. The separation phase can cause the symptoms of flashes. You
may expect the flashes phase to last up to a few months after which they will subside.
The floaters will persist but will become less noticeable as your brain gets used to them.
Can they be treated?
In most instances, floaters are not treated. Your brain simply adapts to their presence and ignores
them.
Occasionally, if floaters become troublesome, an operation called Vitrectomy may be offered. This
is major surgery and has its own risks. You should talk to your doctor and carefully consider this
option.
Can floaters cause further problems?
In 1 % to 10% of patients (depending on the risk factors), floaters can be a sign of a problem called
a retinal tear or a retinal detachment. The likelihood of this particular problem depends on some
risk factors which may or may not be present in your eye.
A retinal tear or a retinal detachment is a serious problem that can cause blindness.
A retinal tear or detachment may require urgent laser treatment or surgical treatment or both. The
urgency depends upon the size of the tear and the amount of retinal detachment.
What should I do if I notice floaters?
You should go to your local eye doctor and have a full eye check up called dilated fundal
examination. Your pupils will be dilated (and vision becomes blurred for a few hours), and then the
doctor will examine your retina and vitreous.
What are the danger signs?
If you notice:
New floaters
Flashing lights
Visual loss
Visual field loss
A curtain falling on your eye through which you cannot see
If you notice any of the above, see your eye doctor immediately.
Seek medical advice if you experience any new eye problems following treatment.
Disclaimer: This information leaflet is produced to help increase awareness regarding floaters. It is not intended to
replace professional medical advice or to provide advice in any special individual circumstance. Please seek expert
medical advice regarding your specific medical condition
Fluorescein & ICG Angiography
Fluorescein angiography is a specialised dye test to discover specific abnormalities
in the retina. A dye, called Fluorescein, is injected into the vein of your arm and
photographs of the back of the eye are taken. The FFA test gives your doctor more
information about the condition of your retina in the back of your eye. ICG test
provides information about the choroid which lies underneath the retina.
The tests help the doctor to consider the best treatment options for you.
Please tell us if you have any chest or breathing problems. It is also very important to
inform us of any allergies particularly to shellfish, medications, fluorescein,
sulpha drugs or latex.
Your vision will be tested. Your pupils will then be dilated with eye drops; these drops
might blur your vision for 3 to 6 hours. It is therefore advisable not to drive home
after your appointment. Once your pupils are dilated, you will be taken into the
fluorescein photography room. You will be seated at a camera with your arm
supported, and some photos will be taken. A cannula (small plastic tube) will be
inserted into a vein. The fluorescein dye will be injected into your arm while a series
of photos are taken as the dye enters the vessels at the back of your eye.
The whole test only takes about 10 – 30 minutes, but please expect to be in the
department for one to two hours so that we can do the necessary pre and post test
checks.
The fluorescein dye will give your skin a yellow tinge and your urine will be bright
yellow for a few days. You might experience a hot flush sensation as the dye is
injected, One in 10 patients might feel nauseous or short of breath, or develop a
transient rash, but this rarely lasts for more than a few seconds. There is a very
remote risk of a severe allergic reaction to these intravenous drugs. For this reason,
an emergency resuscitation team is always available.
The cannula will be left in your hand for half an hour. Once we are certain that you
have not suffered any adverse reactions, the cannula will be removed.
Associated risks with Fluorescein angiography
Fluorescein angiography may be associated with any of the following risks:
Yellow colour change of skin and urine – this affects everyone and lasts 24
hours.
Nausea – may develop 30 seconds or so after injection, but often passes
quite quickly.
Vomiting – rarely follows nausea and again resolves quickly.
Fainting or dizziness
Temporary dazzling
Temporary rose coloured vision
Allergy reactions: These are very rare. The most common allergy reaction is
an itchy skin rash known as hives. In very exceptional circumstances severe
and life threatening allergy reactions can occur resulting in hospitalisation or
even rarely in death. (Risk less than 1 in 50,000).
Associated risks with ICG angiography
Same as above but the dye does not make the skin or urine yellow
ICG angiogram is thought to have less adverse effects than fluorescein
angiogram.
ICG angiogram does not give the same information as the Fluorescein
angiogram therefore sometimes both tests may be necessary
You must not have fluorescein angiography if you are pregnant – please tell your
Doctor.
Please inform your Doctor if you have had any reaction to fluorescein angiography
on a previous occasion.
The doctor will discuss the results with you at your next consultation or will write to
you and your GP and make recommendations for any treatment you might need.
OCT or Retinal scans
What is OCT?
OCT is short for Ocular Coherence Tomography. It is a technology used to scan the
retina, optic nerve, macula, cornea and the irido-corneal angle of the eye. The scan is
non invasive and shows the area of interest in great detail and usually in layers.
Why do I need a scan?
A retinal scan is a great way of finding about retinal diseases that may otherwise
remain undetected if no scan is done. Subtle changes in the retinal structure can be
detected much sooner than the human eye is able to detect. Objective
measurements can also be performed and scans done can show changes from
previously done scans.
When is it used
Retinal OCT scans are usually requested when patients have retinal diseases like
macular degeneration, retinal vein occlusions or diabetic retinopathy.
OCT can also be useful in other retinal conditions which may detect macular odema
or macular pathology.
OCT scans for the optic nerve are used in glaucoma detection or optic nerve
swelling detection.
What does a scan look like
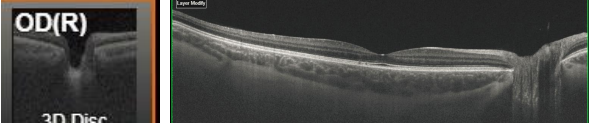
Scan of optic nerve Scan of the retina and macula (Normal)
Disclaimer: This information leaflet is produced to help increase awareness regarding uveitis It is not
intended to replace professional medical advice or to provide advice in any special individual
circumstance. Please seek expert medical advice regarding your specific medical condition
Uveitis / Iritis
What is iritis or uveitis?
The iris is the coloured part of your eye, and iritis simply means that this has become
inflamed. This usually causes misty vision, redness of the eye and a dull ache which is
worse in bright light.
Why have I got iritis?
In many people the cause of iritis is unknown. Sometimes people get iritis in association
with other conditions like arthritis and autoimmune conditions. If you have repeated
attacks, you may have some tests done to see if there is any associated general health
condition.
Can Iritis cause blindness?
Iritis or uveitis can cause loss of sight by several mechanisms. It can cause
cataracts, raised pressure in the eye, damage to the optic nerve, damage to the
retina, extremely low pressure in the eye, and corneal problems. Sight can be lost
permanently by any of these mechanisms. It is therefore essential that you seek
professional help consulting by an eye doctor with a special interest in uveitis.
How is iritis treated?
Most people with iritis respond to eye drops within a few weeks. The drops used are:
(1) Steroids; These drops are given throughout the day as eye drops (such as Maxidex
or Predforte) and at night as a longer action cream (eg, Betnesol). The frequency and
the amount of eye drops is usually determined by your eye doctor keeping in mind the
severity of iritis. As your symptoms improve your doctor will suggest that you gradually
reduce the number of drops you use each day.
(2) Drops to dilate the pupil (such as atropine or cyclopentolate). These make the vision
blurred but usually take the pain away. They are usually necessary in the early stages of
a uveitis / iritis episode and make the eye feel more comfortable. They also reduce the
chances of damaging complications.
Severe Iritis
In severe uveitis, patients may need injections around the eye. These are usually
steroid injections. These can be given in or around the eyeball.
Occasionally patients need steroids in a tablet form. These are usually reserved for
very severe cases of uveitis with retinal complications. The side effects of high dose
oral steroids can be severe, so please ask your doctor if you think that you are
having problems with high dose oral steroids.
Very severe iritis / uveitis
Some patients with very severe uveitis will need oral steroids followed by steroid
sparing agents. These may be drugs like Methotrexate, Infliximab, adalilumab,
cyclosporine and Azathioprine. Sometimes these drugs are also used in cancer
treatments.
Will the iritis come back again?
Iritis tends to recur and it is important that you go to eye unit if your symptoms return,
so that you can be treated promptly.
What are Mr Ijaz Sheikh credentials in treating uveitis?
Mr Ijaz Sheikh has a lot of experience in treating uveitis patients. He runs a weekly uveitis clinic in St
Helier hospital London to treat uveitis patients. He set up the Liverpool Uveitis database and
Liverpool paediatric Uveitis database. He has several publications in the field of uveitis.
Disclaimer: This information leaflet is produced to help increase awareness regarding uveitis
It is not intended to replace professional medical advice or to provide advice in any special
individual circumstance. Please seek expert medical advice regarding your specific medical
condition.
Blepharitis
Blepharitis is a condition where the edges of the eyelids become inflamed (red and
swollen).
It is a common condition, accounting for an estimated 1 in 20 eye problems. Blepharitis
can develop at any age, but is more common in people over 40.
Signs of blepharitis can include:
itchy and sore eyelids
eyelids that stick together and are difficult to open
eyelashes that become crusty or greasy
Blepharitis can be caused
by an infection with bacteria
seborrhoeic dermatitis – (oily or flaky skin)
rosacea – (red and blotchy skin)
Blepharitis is not contagious.
Blepharitis is usually a long-term condition.
Most people experience repeated episodes, separated by periods without symptoms.
Blepharitis cannot usually be cured, but a daily eyelid-cleaning routine that involves
applying a warm compress – gently massaging your eyelids and wiping away any crusts –
can help control the symptoms.
Sometimes antibiotics and mild steroids are needed to treat these. They should be taken
only with consultation with an ophthalmologist. More severe cases may require oral
antibiotics.
Shampooing the eyelids
Taking a mild baby shampoo and shampooing the eyelid margins once or twice a week
may be helpful. Take care not to let any shampoo get in the eye itself and just shampoo
the eyelashes. Remove any crusts if you can.
Warm compresses
Take a warm flannel and apply it to the lids affected for a few minutes. The flannel should
be warm and comfortable. Do not apply a hot flannel to the eyelids. Massage the eyelids
as you keep the warm flannel on the eye. This will help the oily secretions and oily tears to
flow much better.
Disclaimer: This information leaflet is produced to help increase awareness regarding blepharitis. It is not intended to replace
professional medical advice or to provide advice in any special individual circumstance. Please seek expert medical advice regarding
your specific medical condition.
Chalazion
A chalazion is a firm round lump in the upper or lower eyelid caused by a chronic
inflammation/blockage of the meibomian gland. It can sometimes be mistaken for a stye.
Eyelid glands are called the meibomian glands. There are 30-40 of these glands in each of
the upper and lower lids. These glands produce an oily secretion which is mixed into the
tear film of the eye and provides eye surface lubrication. The tiny openings of each of these
oil or sebaceous glands are just behind the eyelashes at the lid margins of both the upper
and lower eyelids.
The narrow opening through which a meibomian gland secretes its material can become
clogged from narrowing of the opening or hardening of the sebaceous liquid near the
opening. This can happen because of dead cells, eyelashes, inflammation or low grade
infections on the eyelid surface. If this occurs, the gland will have a backup of the material it
secretes and the obstructed gland will swell. This leads to thickening of the walls of the
gland and leakage of oil into the lid itself, causing inflammation both within the gland and
the eyelid. This inflamed enlargement is a chalazion.
A chalazion may present as an eyelid swelling or lump, eyelid tenderness or heaviness of the
eyelid. Sometimes, as it presses on the surface of the eye, it can cause blurred vision.
If a chalazion is inflamed, it can cause a red, watering and sore eye
Treatment
Treatment involves cleaning and warm compresses to the eyelid. Apply a warm compress
which can be used to increase drainage of the affected gland. Gently massage after warm
compress to help to express the contents of the cyst.
If acutely inflamed, the patient may need antibiotic ointments and mild steroid drops for a
few weeks. Please contact your doctor who will prescribe this for you if needed.
Upto 50% Chalazia will disappear with the above treatment over the course of a few
months.
If conservative therapy fails, chalazia can be treated by a surgical procedure under local
anaesthetic. This is called incision and curettage. The procedure can take upto 10 minutes
once started. This procedure involves a surgical incision into the tarsal gland followed by
curettage of the retained secretions and inflammatory material under local anaesthetic.
Disclaimer: This information leaflet is produced to help increase awareness regarding chalazion. It is not
intended to replace professional medical advice or to provide advice in any special individual circumstance.
Please seek expert medical advice regarding your specific medical condition.
Dry eye
Dry eye is a common condition that occurs when the eyes do not make enough tears or
the tears evaporate too quickly.
This leads to the eyes drying out and becoming inflamed (red and swollen) and irritated.
The symptoms of dry eye syndrome usually affect both eyes and often include:
feelings of dryness, grittiness or soreness that get worse throughout the day
red eyes
eyelids that stick together when you wake up
temporarily blurred vision, which usually improves when you blink
Dry eye syndrome can occur when the complex tear production process is disrupted in
some way. There are many different reasons why this can happen, although a single
identifiable cause is not often found.
Common causes include:
being in a hot or windy climate
wearing contact lenses
certain underlying medical conditions, such as blepharitis (inflammation of the
eyelids)
side effects of certain medications
hormonal changes, such as during the menopause (when a woman’s periods stop)
Although the condition can affect people of any age, your chances of developing dry eye
syndrome increase as you get older. It’s estimated that up to one in every three people
over the age of 65 experiences problems with dry eyes.
Dry eye syndrome is also more common in women than men.
Dry eye syndrome is not usually a serious condition.
Treatments are available to help relieve the symptoms, which include eye drops to
lubricate the eyes, medications to reduce any inflammation, and (if necessary) surgery to
prevent tears from draining away easily.
If dry eye syndrome is caused by an underlying condition, treating this condition will
usually help relieve the symptoms.
As well as medical treatments, there are some things you can do yourself to help prevent
dry eye syndrome or reduce the symptoms.
These include:
keeping your eyes and eyelids clean and protecting them from dusty, smoky, windy
and dry environments
using your computer or laptop correctly to avoid eye strain
using a humidifier to moisten the air
eating a healthy diet that includes omega-3 fats
Dry eye syndrome may be uncomfortable, but does not usually cause any serious
problems. In rare cases, severe untreated dry eye syndrome can cause scarring of the
eye’s surface, leading to visual impairment.
Contact your GP or visit your nearest accident and emergency (A&E) department
immediately if you have any of the following symptoms, as they could be a sign of a more
serious condition:
extreme sensitivity to light (photophobia)
very red or painful eyes
a deterioration in your vision
Disclaimer: This information leaflet is produced to help increase awareness regarding blepharitis. It is not intended to replace
professional medical advice or to provide advice in any special individual circumstance. Please seek expert medical advice regarding
your specific medical condition.
Laser Peripheral Iridotomy
Glaucoma is a lifelong disease where a high pressure inside the eye results in damage to the
optic nerve and loss of vision. It cannot be cured but can, in most people, be controlled. The
pressure inside the eyeball depends on production of a clear fluid (called aqueous humour)
which circulates through the eye and drains out of the natural drainage system called the
trabecular meshwork.
In some patients, this drainage system will be affected if the front part of the eye is narrow.
Sometimes in some patients this drainage site may be totally closed leading to a sharp rise of
the intraocular pressure causing severe eye pain, vomiting and sometimes abdominal pain. This
leads to permanent and irreversible loss of sight if untreated. Laser peripheral iridotomy reduces
the risk of this by creating a hole in the iris to bypass the closure and reduce the pressure in the
eye.
The Procedure
Peripheral Iridotomy is performed in the laser clinic. The laser treatment itself takes
approximately 10 minutes per eye. You will need a one-off dose of eye drops, including
Pilocarpine 2% eye drops, approximately 15 minutes beforehand, so be prepared for an
appointment lasting an hour. The drops can blur your vision slightly and some patients report a
slight headache after use.
The procedure involves a machine much like the one used in the main clinic. A local
anaesthetic eye drop is used to allow a contact lens to be positioned on the eye. This will be
held in place by the doctor performing the procedure and is removed at the end of procedure.
The treatment does not hurt and afterwards the eye may be somewhat dazzled by the bright
light but this will fully resolve within 30 minutes.
Usually one eye is done at a time and sometimes one eye may need more laser power that the
other eye, this is normal.
After the procedure
After the treatment, a single eye drop will be administered by your doctor to prevent a transient
rise in your intraocular pressure. You will be given a prescription for a week long course of antiinflammatory eye drops to be used 3 -4 times per day. Depending upon circumstances, you will
be seen in the Clinic usually 1 week after the procedure.
A letter will be sent to your GP explaining the treatment you have had and details of your followup appointment.
Dos and Don’ts after laser peripheral iridotomy
Watch television, read and write as normal.
Go back to work should you need to, although be aware that the Pilocarpine eye drop used
might blur your vision slightly.
Don’t restrict your physical exertion, there is no need
Don’t be concerned if your vision is markedly affected immediately after the treatment – this is
normal and is due to the bright light used. It will settle spontaneously within 30 minutes to 24
hours.
Risks of peripheral iridotomy
No medical procedure is entirely risk-free but YAG Peripheral Iridotomy has very few side
effects or complications.
Transient pressure rise post-procedure – as mentioned above, an eye drop will be
administered by the doctor performing your procedure immediately before and afterwards
to prevent this
Inflammation – a certain amount of inflammation is required for the treatment to work but
you will be given a prescription for some anti-inflammatory eye drops to settle things down
after the treatment.
Sometimes treatment can cause a transient small amount of bleeding – usually controlled
by slight increase of pressure of the contact lens to stop bleeding.
The treatment is usually only done once – rarely laser treatment may need to be repeated
on another day to achieve full thickness hole in the iris.
Laser iridotomy reduces the risk of acute angle closure glaucoma and therefore sight loss.
The risk is not reduced to zero. It is therefore possible to get acute glaucoma even in an
eye that has been adequately treated.
____________________________________________________________________________
Disclaimer: Medical information is merely information – not advice. If users need medical
advice, they should consult a doctor or other appropriate medical professional. No warranties
are given in relation to the medical information supplied on the website, and that no liability
will accrue to the website owner in the event that a user suffers loss as a result of reliance
upon the information.
Punctal plugs
Punctal plugs are tiny devices inserted into tear ducts to block drainage of tears. This increases
the eye’s tear film and surface moisture to relieve dry eyes.
Also known as punctum plugs, lacrimal plugs or occluders, these devices often are no larger than
a grain of rice.
Punctal plugs usually are considered when lubricating eye drops fail to relieve your dry eye
condition.
How are punctal plugs inserted in tear ducts?
Many eye doctors need only a lighted, close-up examination of your eye to determine the size
and type of punctal plug you need. In some cases, a one-size-fits-all style of punctal plug may be
used. In others, a sized punctal plug will be needed.
To prepare you for the procedure, some eye doctors use a local anesthetic drop before inserting
the punctal plug. In many cases, no anesthetic is needed.
Each eyelid has one punctum, located at its inner margin near the nose. Punctal plugs can be
inserted in the puncta of the lower lids, the upper lids or both. An instrument may be used to
dilate the tear duct opening for easier insertion.
Many punctal plugs are pre-packaged with disposable devices that help your eye doctor insert
the plug. Some punctal plugs are inserted just into the puncta so they still can be seen and
mechanically removed if necessary.
Other than slight initial discomfort, you should not feel the punctal plug once it is in place.
Immediately after the procedure, you should be able to drive yourself home and resume normal
activities.

Punctal plugs side effects and problems
Usually, punctal plug insertion is uneventful and rarely involves serious side effects or problems.
Excessive tearing (epiphora) and watery eyes can occur when the punctal plug does its job too
well. In this case, you may need to visit your eye doctor for removal of the plug or replacement
with a different type to better control the amount of tears on your eye.
Displacement or loss of the plug is common and can occur for many reasons, such as when
people rub their eyes and accidentally dislodge the device. Some types of punctal plugs in
particular are more likely to become dislodged and fall out. You will need to visit your eye doctor
to receive a replacement punctal plug.
Eye infections may occur, though rarely, in association with the devices. In these cases, you may
need treatment with topical antibiotics, oral antibiotics and/or removal of the punctum plug.
Other uncommon complications can occur when the plug unexpectedly migrates outside the
target area and deeper into the eye’s drainage channels. This can create blockages leading to
conditions such as dacryocystitis, with swelling, pain and discomfort.
When should punctal plugs be removed?
While semi-permanent punctal plugs can last indefinitely, they also are easily removed.If you get
excessive tearing and you feel that you no longer need them , they can be removed.
Dilation of pupils
When seeing an eye doctor, it is sometimes necessary to examine the retina. In occasional
cases, the doctor may be able to look through the pupil and examine the retina and the optic
nerve if your pupil is naturally large. However in most cases and especially if the doctor needs to
see your peripheral retina (at the back of your eye), eye drops may need to be put in to dilate the
pupil.
Looking through the pupil is like looking through a keyhole. If the keyhole is small it will be
difficult to see whats on the other side. If the keyhole is large, it will be easier to see and it will be
possible to see more on the other side. If the pupil is large, it becomes easier to see the retina
and also more of the retina can be seen by the doctor.
Doctors will usually prescribe and then put in drops called 2.5% phenyl epinephrine and 1%
tropicamide eye drops. Occasionally trained optometrists and nurses may also have
qualifications to put in these eye drops. The drops can sting for 1-2 minutes but afterwards the
eye becomes comfortable.
After 10 to 15 minutes, the pupil usually dilates. The duration it takes to dilate can be very
variable with some people having a dilated pupil in 5 minutes and in some other people it can
take as long as 30-40 minutes.
People usually feel that the near vision becomes blurred after the pupil dilates. The effect can be
variable and some people feel distance vision is blurred as well.
After the doctor has examined the eye you can go home. Do not drive until you feel that your
vision is good enough. It’s usually a good idea for someone else to drive and take you home.
The pupil will usually take 3-6 hours to come back to its proper size and reactive state. Again the
duration can be variable depending upon the individual. Some people will have minimal problems
and the vision will return to normal within an hour or two. In others, visual blurring may persist for
5-6 hours. It is unusual for visual blurring to persist for more than 6 hours.

Very few people (less than 1%) may develop significantly raised pressure in the eye after pupil
dilation. If this happens, patients may experience pain, redness and blurred vision. In this case,
the doctor should be contacted immediately.
Disclaimer: Medical information is merely information – not advice. If users need medical advice,
they should consult a doctor or other appropriate medical professional. No warranties are given in
relation to the medical information supplied on the website, and that no liability will accrue to the
website owner in the event that a user suffers loss as a result of reliance upon the information.
Conjunctivitis
Conjunctivitis means inflammation of the conjunctiva.
This usually means a red eye.
There are a lot of causes of a red eye and conjunctivitis is one of them.
There may be many types of conjunctivitis –
Allergic conjunctivitis – caused by allergies and can cause a red eye off and on for months to
years
Bacterial conjunctivitis – caused by bacteria and can cause a sore red eye with discharge and
swelling. This may require antibiotic drops.
Viral Conjunctivitis – caused by viruses and results in a sore red eye with watery discharge and
swelling. This is not helped by antibiotic drops. It can spread very quickly to other members of
the family or anyone who is in contact with the patient.
You must go to your eye doctor and a slit-lamp examination.
This will help diagnosing the subtype of conjunctivitis and treat it appropriately as treatment of
each of these subtypes is radically different.
General precautions in helping the spread of infectious conjunctivitis (bacteria or viral)
1. Wash hands frequently specially before putting in eye drops
2. Keep hand towel separate and do not let other members of the family use it
3. Do not touch the unaffected eye
4. Use tissues and then throw them away in the bin ( disposable tissues)
5. Change pillowcases frequently and don’t let other members of the family use your pillow
Disclaimer: Medical information is merely information – not advice. If users need medical advice,
they should consult a doctor or other appropriate medical professional. No warranties are given in
relation to the medical information supplied on the website, and that no liability will accrue to the
website owner in the event that a user suffers loss as a result of reliance upon the information.
